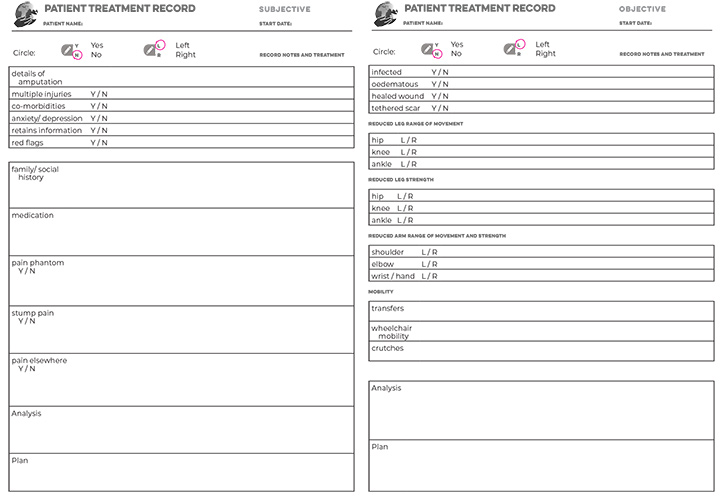
Patient records
(S O
O A
A P)
P)
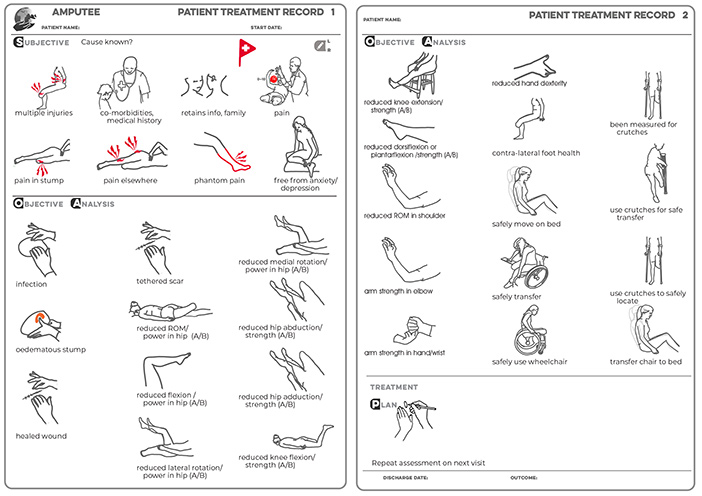


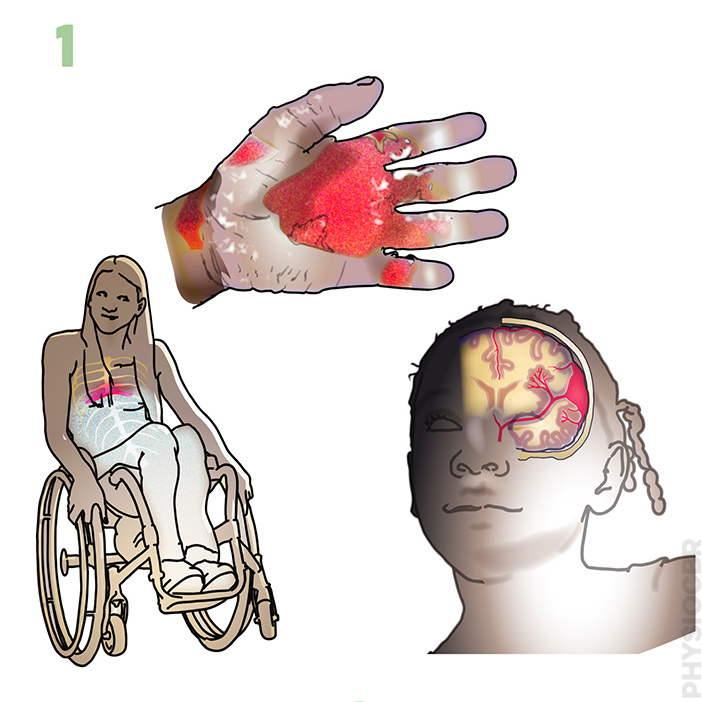 1. Multiple injuries
1. Multiple injuries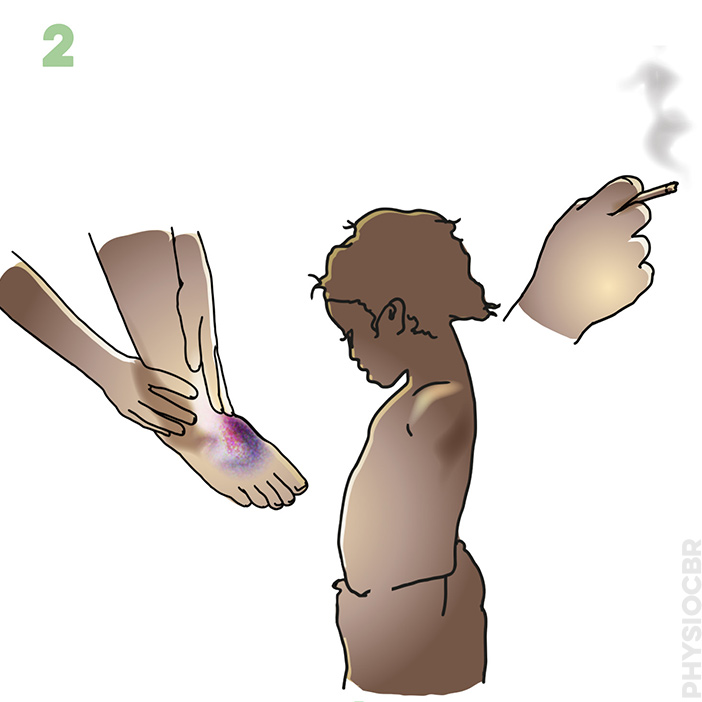 2. Co-morbidities
2. Co-morbidities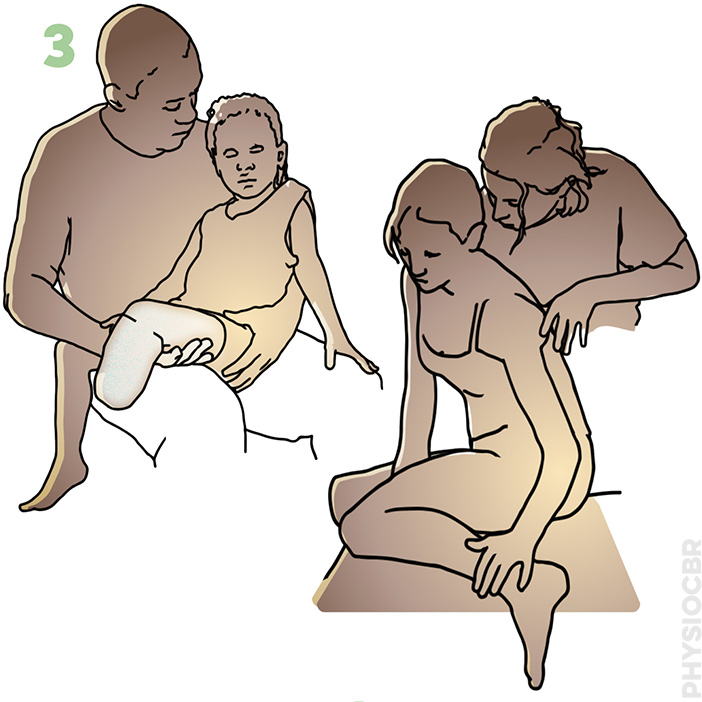 3. Readiness to learn
3. Readiness to learn 5. Pain
5. Pain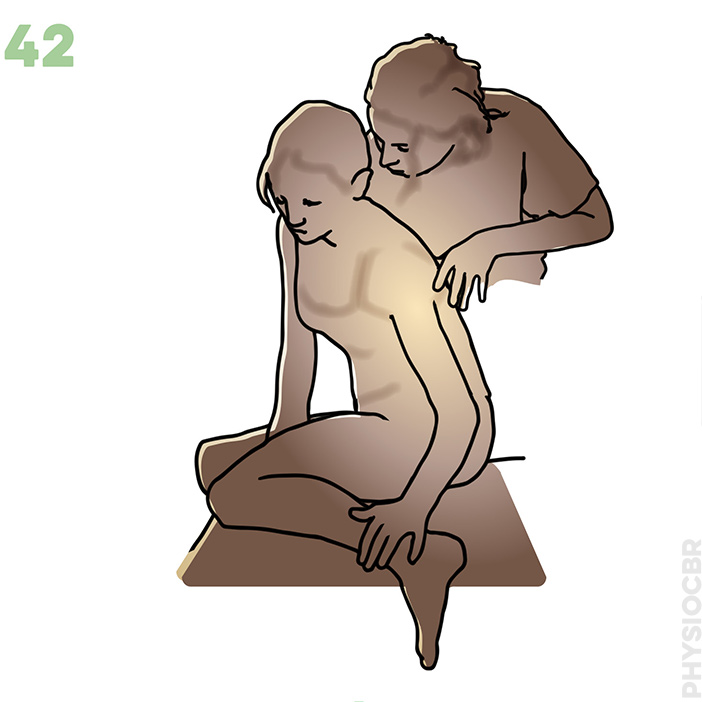 15. Anxiety/ depression
15. Anxiety/ depression









S.O.A.P. notes make your assessment and treatment logical and keep your records clear.
S = Subjective; what the patient tells you i.e. symptoms you cannot see such
as pain or how they are feeling, and details
about family or living conditions
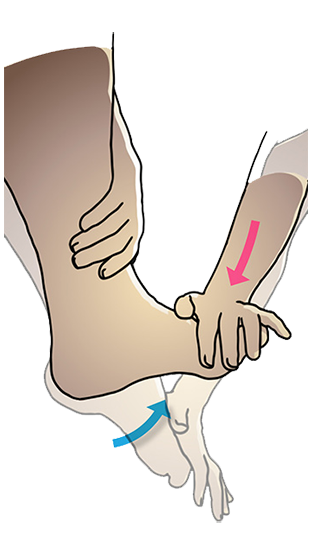
O = Objective; what you see (e.g. signs of infection or range of movement) and what you do (treatment given)
A = Analysis: what might be happening, e.g. show clinical reasoning
P = Plan: what you want to do next time, such as add a new treatment as
patient progresses
When you are ready, please proceed to the assessment of your patient.